You are here
Root Canal Treatment

Root canal treatment is part of the Endodontic discipline within dentistry. It is also the most commonly performed procedure within this discipline. Endodontic basically deals with the tooth pulp and the tissues surrounding the root of a tooth.
Root canal treatment is usually performed when the pulp (containing mostly nerves, blood vessels and lymphatic tissue) has become diseased or injured, and cannot repair itself, therefore starts dying. Root canal treatment allows the tooth to be saved, instead of being removed.
The most common disease that can lead to a root canal treatment is caries (tooth decay) that has progressed far into a tooth, all the way into the pulp itself.
Caries is the result of excessive exposure to sugar and/or acid, resulting in the loss of enamel mineral, eventually leading to the collapse of the whole enamel matrix in the region, forming a "hole". More often than not, it is not the absolute amount of sugar that one consumes that matters, but the frequency of exposure to the sugar and acid attack.
Sugar = any sugars added, or food/drinks being digested and broken down into a form of sugar substrates (eg. carbohydrate into sucrose, milk into lactose, fruit into fructose)
Acid = acid from any carbonated drinks, or as a byproduct of bacterial fermentation of sugar substrates in the mouth
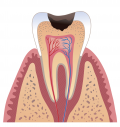
 Cross sectional view of a healthy tooth. Outer most layer is enamel, then dentine, then the pulp right in the centre with blood and nerve supplies entering the tooth via the apex of the root.
Cross sectional view of a healthy tooth. Outer most layer is enamel, then dentine, then the pulp right in the centre with blood and nerve supplies entering the tooth via the apex of the root.
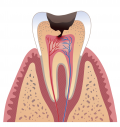
 Caries (decay) starting in the enamel layer. Usually no filling required if the surface has not cavitated (collapsed).
Caries (decay) starting in the enamel layer. Usually no filling required if the surface has not cavitated (collapsed).
 Caries entering into the dentine layer. Filling is required by this stage.
Caries entering into the dentine layer. Filling is required by this stage.
 Caries has entered the pulp. If the exposure point is very tiny, it may be possible to simply do a filling and the pulpal tissue may repair itself. However the tooth is likely to need root canal treatment in the future.
Caries has entered the pulp. If the exposure point is very tiny, it may be possible to simply do a filling and the pulpal tissue may repair itself. However the tooth is likely to need root canal treatment in the future.
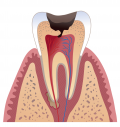 Caries has entered the pulp and inflammation is well established in the pulp chamber, sometimes even all the way down the canal, causing an abscess to develop at the apex of the root. Root canal treatment is the only way to save and keep the tooth. The alternative will be extraction (removing the tooth).
Caries has entered the pulp and inflammation is well established in the pulp chamber, sometimes even all the way down the canal, causing an abscess to develop at the apex of the root. Root canal treatment is the only way to save and keep the tooth. The alternative will be extraction (removing the tooth).
Other causes that can result in the infection or inflammation of the pulp include:
- a very deep cavity/filling
- repeated dental work to the tooth
- trauma (be it accidental trauma or from having a traumatic occlusion/bite)
- gum disease
- a crack in the tooth that has propagated through to the pulp
- extreme wearing down of the tooth through grinding +/- acid erosion.
Symptoms commonly include pain, increased/decreased sensitivity to heat or cold or pressure (depending on the stages of pulpal death), tooth discolouration, and swelling (abscess) in the surrounding gum.
What are the benefits of saving the tooth with a root canal?
Generally speaking, the tooth
- will function better than a replacement, artificial tooth (be it denture, bridge or implant)
- is stronger and more efficient in chewing (despite root canal treated tooth do gradually become relatively more brittle than a vital tooth)
- can be cleaned and maintained easier
What if the tooth is removed and no artificial replacement is sought?
Adjacent teeth can move and drift out of their normal position, changing the bite (occlusion). In more severe cases, especially when multiple teeth are missing, this may lead to jaw joint malfunction and pain.
Adjacent teeth can also gradually tilt so much that it becomes rather difficult to brush around them efficiently, making them more prone to gum disease +/- decay, and therefore potentially further tooth loss.
What about the success rate of root canal treatment?
It is good. The success rate is usually above 90% (up to 99%) depending on the timing of treatment, the expertise of the treating clinician and the long term care of the tooth. If well taken care of, the tooth often lasts for many years, and possibly even for life.
What about the risk or side effects of root canal treatment?
- Loss of the tooth --- despite the best effort of the clinician, success and healing depend on the patient's age, general health, healing ability, timing of treatment being commenced, severity of infection, timing of final restoration placement etc. No one can actually guarantee that a root canal treatment will be successful.
A commonly neglected factor (by the patient) is the timing of final restoration placement. Delay in doing so can result in bacteria re-entering the root canal system, causing a new infection.
Another common factor is the delay in completing the whole treatment as advised, especially when pain has been removed by the initial dressing. This may lead to a chronic infection, which at times may get out of hand so much that the tooth simply will not settle down and extraction is the only option.
- Tooth discolouration --- often happens gradually over the years, losing its original colour and becoming darker. However the situation can be improved by bleaching (often in the form of internal bleaching), or placing a crown or veneer to mask the discolouration.
- Altered sensation --- A root canal treated tooth, particularly a molar (back) tooth, may feel "different" or "weaker" when compared to the other teeth. Usually it is most noticeable during and immediately after treatment, then gradually disappear. However some people do find the altered sensation rather persistent, while others may find that they can feel it only when their general immune systems are down.
- Re-treatment --- usually required due to further new decay, trauma or a crack in the filling, allowing bacteria to re-enter the root canal system, causing another infection. Time frame can range from months to years after the initial treatment.
- Pain or discomfort --- can sometimes persist during and following each treatment appointment. Analgesics may be recommended. Often also indicates that further treatment to the tooth will be required, especially if the pain is severe or lasts more than a few days.
So what exactly does the root canal treatment involve?
- removing all decayed tooth structure
- creating full access to the pulp via the biting surface of the tooth
- cleaning out any remnant tissues within the pulp and the root canals (all canals must be treated, usually with anterior teeth having only 1 canal, premolars 1 - 2 canals, molars 3 - 4 canals)
- enlarging and shaping the canals in preparation for special root canal filling
- placement of antibacterial medicaments (leave in in-between appointments) into the canals and pulp to clear out the very fine dentinal tubules not accessible by the dental instruments
- inserting the special root canal filling when all canals are clean and shaped, and the tooth is symptom-free
- then the final restoration to seal up the root canal filling --- could be a simple composite or amalgam filling, or sometimes a crown may be recommended as well.
- On average, the root canal treatment often takes 3 - 5 appointments over several months.
Other procedures practiced within Endodontics include retrograde root filling, incision for drainage, apicectomy (root-end resection), apical curettage, hemisection, root resection and intentional replantation. These more radical/invasive treatments are generally required only in cases of abscesses, root fractures, and problematic tooth anatomy, but may also be indicated in treating teeth that have persistent root end pathology following conventional root canal treatment.
Our Doctors
Opening hours
- Monday: 9am–5pm
- Tuesday: 9:30am–6pm
- Wednesday: 9am–5pm
- Thursday: 9am–5pm
- Friday: 9am–5.30pm
- Saturday: 9am–1pm
- Sunday: Closed

